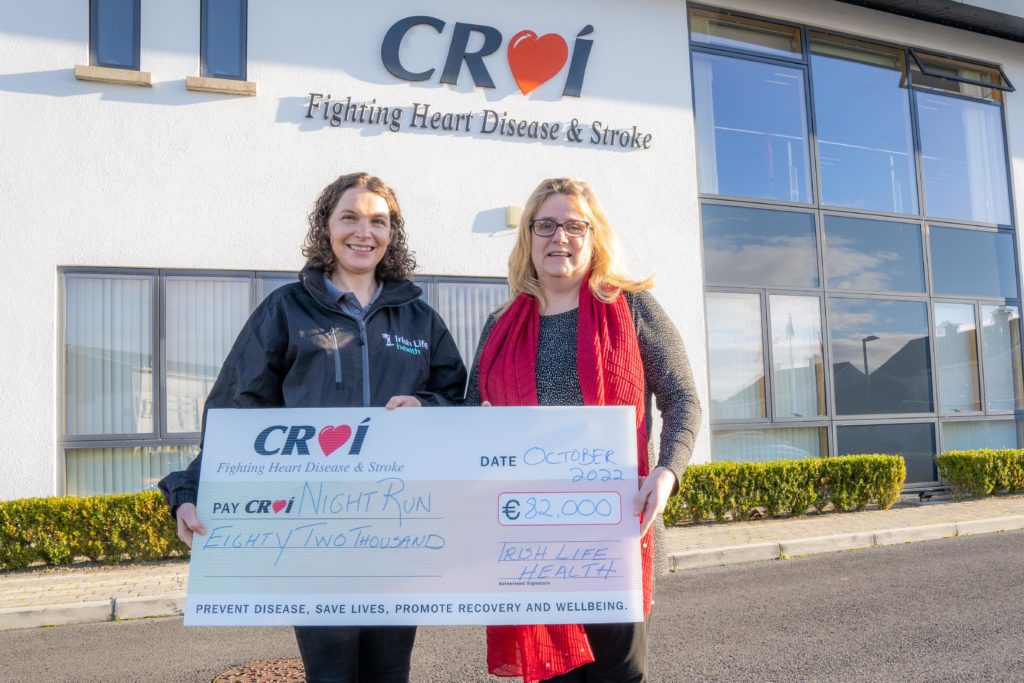
Croí’s 2022 Night Run raises 82k!
Presenting a cheque for €82,000 from the 8th Annual Croí Night Run, is Edel McDermott – Key Account Manager, Irish Life Health to Christine Flanagan, Croí’s Director of Fundraising. With […]
Croí’s 2022 Night Run raises 82k! Read More »